The definition of SBAR comes from its acronym, “Situation, Background, Assessment, Recommendations.” It’s the best practice for nurses to communicate info to physicians and other health professionals. In this article, you’ll find an explanation of how and when to use this standardized communication tool. You’ll also find an SBAR PDF form for use in any healthcare communication situation.
What is SBAR?
SBAR is a standard way to communicate medical info. It improves accuracy and cuts down on dangerous errors.
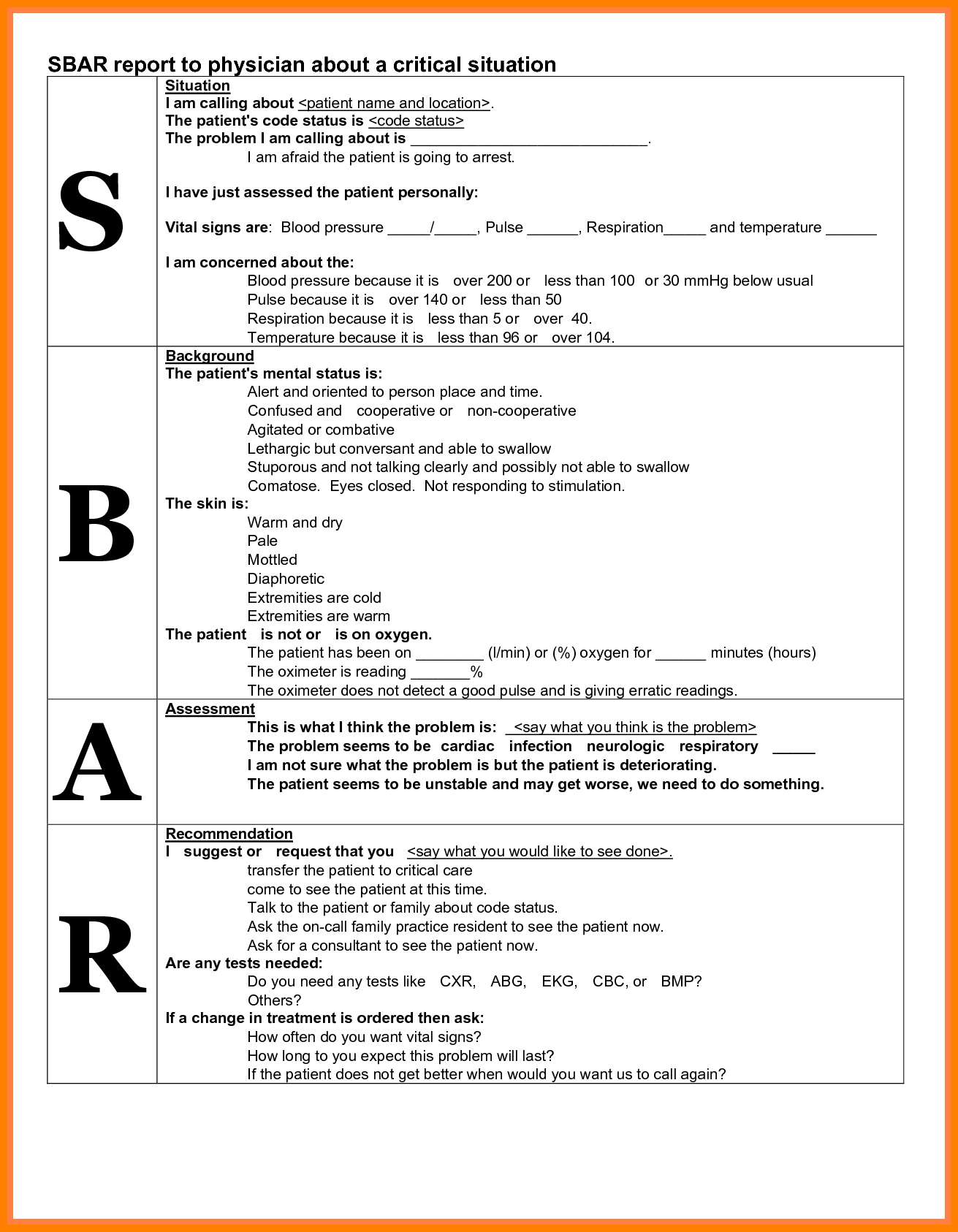
SBAR stands for:
- Situation
- Background
- Assessment
- Recommendations
The above terms represent the four key facts that must be conveyed.
SBAR is a standardized, safe, simple way for nurses and doctors to share patient information in a sharp, clear way.
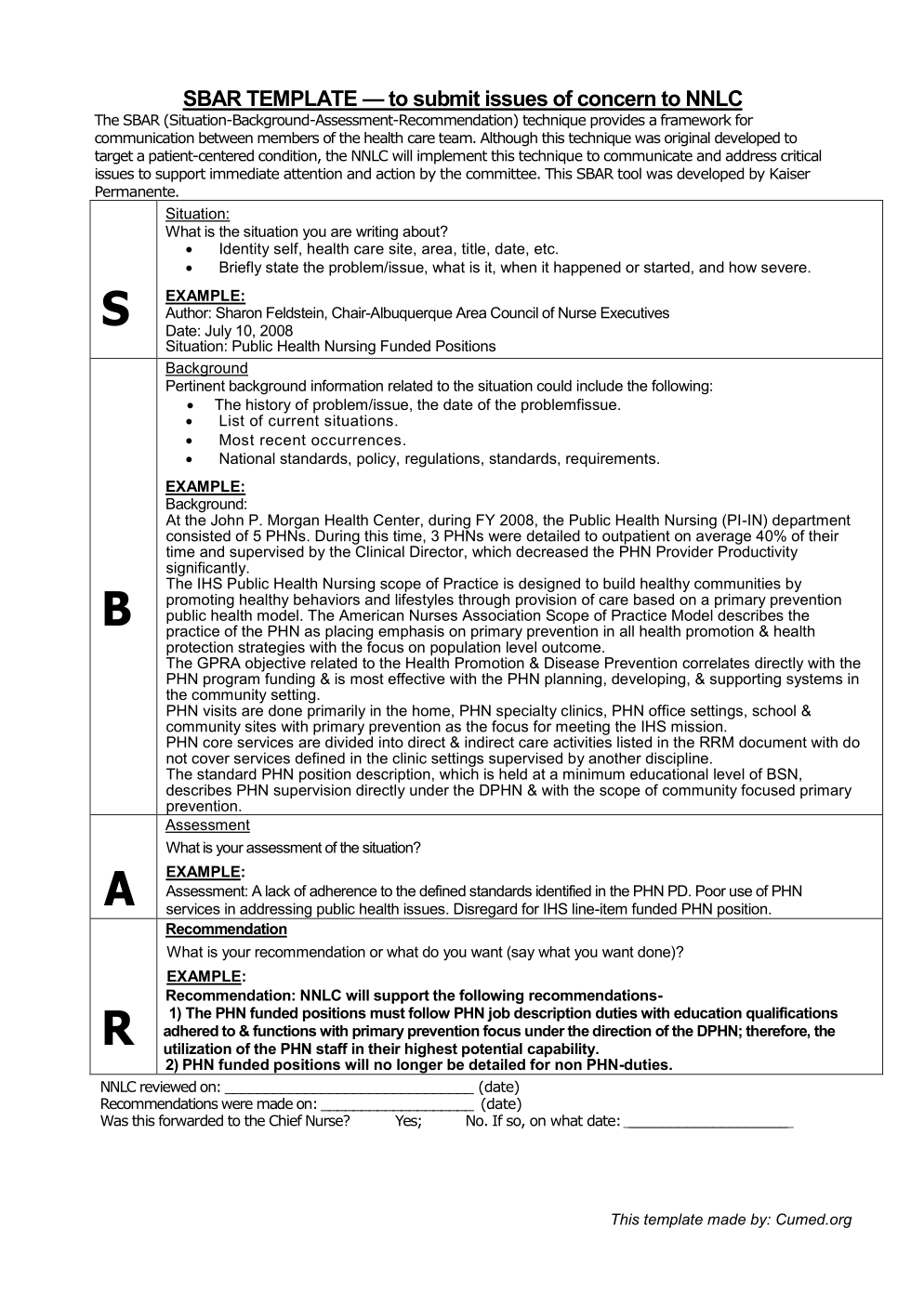
Sbar Format – Google Search | Nursing | Sbar, Sbar Nursing – Sbar Template Word
Download PDF: Click Here
Download Word: Click Here
Why Use SBAR?
In a word: accuracy.
SBAR is endorsed by the Joint Commission as the best practice for communication for physicians and nurses.
The Joint Commission endorses SBAR as an easy-to-use tool to improve communication. According to the Commission, the tool lets nurses send a complete message to doctors concerning a patient’s condition.
Because information is given in a standardized way, there’s less room for human error. This greatly improves accuracy.